For my own personal use only:
-
Heart failure
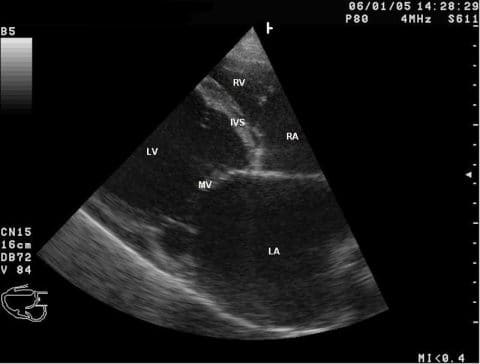
Echocardiogram of dog with dilated cardiomyopathy showing marked left atrial and left ventricular dilation - Classic case:
- Cough, exercise intolerance
- Abdominal distension
- +/- Heart murmur or arrhythmia
- Harsh lung sounds/crackles
- Dx:
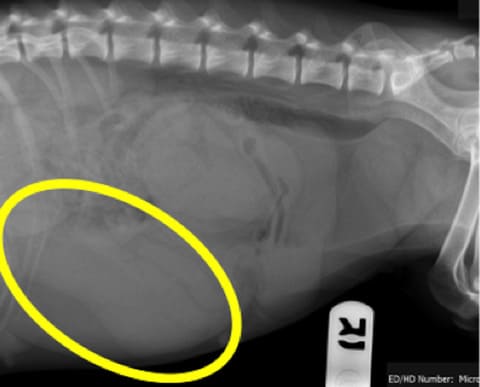
- Thoracic radiography shows:
- Heart enlargement
- Dilated pulmonary veins
- Interstitial to alveolar lung changes in caudodorsal lung fields
- Echocardiography shows:
- Left atrial +/- left ventricular enlargement (causing pulmonary edema)
- +/- Poor contractility
- Valvular insufficiency
- Right atrial and ventricular dilation (causing ascites)
- Thoracic radiography shows:
- Tx:
- Acute:
- Diuretics: furosemide
- Oxygen therapy (cage or nasal cannula)
- Positive inotrope and vasodilator: pimobendan
- Decrease stress, mild sedation if needed
- Chronic:
- Diuretics: furosemide
- Positive inotrope and vasodilator: pimobendan
- ACE-inhibitor
- Restrict exercise and dietary salt
- Acute:
- Pearls:
- Prognosis is guarded
- Classic case:
- Heartworm
- Classic case:
- Cough and exercise intolerance
- Abdominal distension
- Weight loss/poor body condition
- Dx:
- Annual screening with antigen SNAP test
- Detects protein secreted by adult female worm 5 mos post-infection
- False negatives if:
- Antigen/antibody complex formation
- No adult female worms (e.g., immature females or males only)
- Light parasite load
- Microfilaria test: recommended annually
- Types of tests:
- Modified Knotts
- Filter test
- Direct smear of anti-coagulated blood
- Types of tests:
- Thoracic radiography shows:
- Enlarged, tortuous, +/- blunted pulmonary arteries
- Pulmonary parenchymal disease
- Right heart enlargement
- Echocardiography shows:
- Pulmonary artery dilation
- Right heart dilation
- Visible heartworms in pulmonary artery
- Caval syndrome: heartworms visible in right ventricle +/- right atrium
- Annual screening with antigen SNAP test
- Tx:
- Doxycycline
- Daily, 30 d prior to adulticide
- Heartworm prevention: macrocyclic lactones
- Prevent new infections
- Eliminate susceptible larvae and microfilaria (pretreat with diphenhydramine and corticosteroids if microfilaria positive)
- Treat monthly, starting 2 mos prior to adulticide
- Adulticide: melarsomine dihydrochloride
- 3-dose protocol: IM once, wait 1 mo, then 2 doses given 24 h apart
- Kills 98% of heart worms
- STRICT exercise restriction during adulticide therapy and continuing for 6-8 wks after final dose
- Corticosteroids
- Tapering anti-inflammatory dose to control clinical signs of pulmonary thromboembolism
- Start 1-2 mos prior to adulticide if symptomatic or microfilaria positive
- Surgical extraction of adult worms
- Indicated for dogs with caval syndrome
- Doxycycline
- Pearls:
- Prognosis:
- Good to guarded depending on severity
- Poor to grave for caval syndrome
- Doxycycline therapy to reduce Wolbachia (intracellular bacteria essential for worm survival) makes worms more susceptible to adulticide therapy
- 7% of infected dogs are negative on SNAP and positive for microfilaria
- Prognosis:
- Classic case:
- Pyometra
- Classic case:
- Intact middle-aged female 3-4 wks past estrus
- +/- Mucoid, purulent, or hemorrhagic vulvar discharge
- Polyuria/polydipsia
- Vomiting, anorexia, abdominal pain
- Enlarged, palpable uterus
- Dx:
- Abdominal radiography: distended, tubular, enlarged, fluid-filled uterus
- Vaginal cytology: degenerative neutrophils +/- phagocytized bacteria
- Abdominal ultrasonography: enlarged fluid-filled uterus; differentiates from pregnancy
- Tx:
- Stabilization:
- IV fluids
- Broad-spectrum antibiotics
- Analgesics
- Surgical:
- Ovariohysterectomy is Tx of choice for all animals not intended for breeding
- Medical:
- Option for young breeding animals
- Referral recommended
- Stabilization:
- Pearls:
- Prognosis: guarded to good if uterus is intact
- Rule out pyometra in any systemically ill intact female
- Classic case:
- Flea allergy dermatitis
(FAD)
- Classic case:
- Acute onset of moderate to severe pruritus
- More common in warmer seasons but can be year round
- Excessive self-grooming and hair loss, especially rear half of body
- +/- Visible live fleas
- Dx:
- History and physical exam
- Flea comb to find fleas/flea dirt
- Positive response to flea eradication
- Tx:
- Acute:
- Tapering dose of corticosteroids for pruritus
- Topical/oral flea adulticide
- Chronic:
- Ongoing use of oral/topical flea adulticide
- Oral monthly flea development inhibitors (lufenuron)
- Environmental control: frequent vacuuming, removal of outdoor organic debris
- Acute:
- Pearls:
- Prognosis is good with long-term management
- 15% of dogs do not have evidence of fleas
- Classic case:
- Lameness overview: hip dysplasia, panosteitis, osteochondrosis dissecans (OCD), hypertrophic osteodystrophy (HOD), Legge-Perthes disease
- Classic case:
- Hip dysplasia: "bunny hopping" gait, lameness, difficulty rising, positive Ortolani sign (hip laxity)
- Panosteitis, HOD, OCD: young, medium to giant breeds, more
common in males, acute lameness, fever
- Panosteitis: long bone pain
- HOD: swollen and warm distal limb, metaphyseal pain
- OCD: joint effusion, decreased range of motion
- Legge-Perthes disease (avascular necrosis of femoral head): 3- to 12-mo-old small or toy breeds, pelvic limb lameness
- Dx: Radiography
- Hip dysplasia:
- Shallow acetabulum
- Flattening of femoral head
- Over 50% of femoral head covered by acetabular rim
- Thickened femoral neck
- Panosteitis: multiple long bones have increased medullary opacity, periosteal new bone
- HOD: double physeal line
- OCD: (can use CT)
- Flattening of subchondral bone, joint mouse, joint effusion
- Always image both limbs
- Legge-Perthes disease: loss of bone opacity at femoral epiphysis, moth-eaten appearance of femoral neck and head
- Hip dysplasia:
- Tx:
- Hip dysplasia:
- Surgical: triple pelvic osteotomy, femoral head ostectomy, total hip replacement
- Medical: NSAIDs, weight loss, joint supplements
- Panosteitis, HOD: analgesics
- OCD: surgical debridement or medical Tx with joint supplements and analgesics
- Legge-Perthes disease: surgical femoral head ostectomy or total hip replacement, analgesics
- Hip dysplasia:
- Pearls:
- Hip dysplasia: PennHIP method is more accurate for Dx at an earlier age than OFA method
- Panosteitis, HOD: prognosis is excellent but flare-ups may occur, repeat radiography may be necessary to diagnose
- OCD: prevent by avoiding excessive food and calcium and vitamin D supplements
- Legge-Perthes disease: prognosis with surgery is good to excellent
- Classic case:
Images courtesy Dr. Laura Cousins (heartworm microfilaria, pyometra radiograph, hip dysplasia radiograph), Kalumet (echocardiogram), and Caroldermoid (FAD).
Top Topic Category
Canine