For my own personal use only:
- Presentation:
- Subtle changes in weight-distribution during gait (e.g., mild proximal suspensory strain)
- Non-weight bearing lameness that causes severe distress (e.g., fracture)
- Severe mechanical lameness without pain (e.g., fibrotic myopathy)
- Differentials:
- Traumatic:
- Fracture
- Soft-tissue injury
- Laminitis
- Foreign body
- Bruised sole/heel
- Muscle strain
- Hygroma
- Osteoarthritis
- Congenital:
- Osteochondrosis (or osteochondritis dissecans)
- Angular limb deformity
- Infectious:
- Foot abscess
- Septic joint, tendon sheath, or bursa
- Cellulitis
- White line disease, thrush, quittor, canker
- Lyme disease
- Metabolic:
- Laminitis
- Myopathy
- Mechanical:
- Stringhalt
- Fibrotic myopathy
- Intermittent upward fixation of patella, delayed patellar release
- Circulatory/other:
- Laminitis
- Navicular syndrome
- Improper hoof balance/shoeing (esp. on top of poor conformation)
- Silicosis
- Osteoarthritis
- Keratoma
- Traumatic:
- History:
- Thorough history includes these important
questions:
- Duration?
- Onset (e.g., sudden, gradual)?
- Any previous lameness or recent illness (a high fever etc. might lead to laminitis)?
- Treatments/management of this lameness and results?
- Level of work?
- When was last shoeing/trim?
- What exacerbates it?
- Thorough history includes these important
questions:
- Examination:
- WATCH the horse move:
- Observe from front, side, and behind
- Walk, trot, +/- canter
- In a straight line, +/- on a lunge line
- On hard and soft surface
- In hand or under saddle
- A good exam often takes considerable time depending on severity of lameness
- AAEP lameness scale (1-5): Used by all
practitioners in the US
- Only perceptible under certain conditions (e.g., under saddle, cantering on a certain lead, doing specific movements)
- Consistently perceptible under certain circumstances (e.g., a circle at a trot)
- Constistently perceptible in a straight line and circle at a trot
- Consistently perceptible at a walk
- Non-weight bearing
- Forelimb lameness: Remember "DOWN ON SOUND"
- Head bobs up when lame limb strikes the ground
- Head goes down when sound leg strikes the ground
- Hindlimb lameness: More difficult to assess
- Sacrum/pelvis hikes up (or moves more) when lame limb strikes the ground and falls when the sound limb strikes the ground
- Can get contralateral head bob with severe hindlimb lameness
- Palpation:
- Limbs, joints, soft tissues, neck, back, and musculature
- Look for heat, pain, swelling, effusion
- Compare with contralateral limb
- Observation:
- Muscular asymmetries
- In a horse with multifocal neuro signs, asymmetric muscle atrophy may be suggestive of equine protozoal myeloencephalitis (EPM)
- Watch stride length - often shortened in lame leg
- Wounds or scars
- Stance at rest
- Wear on hooves/shoes and hoof conformation
- Muscular asymmetries
- Flexions: To help localize source of lameness
- Distal forelimb, carpus, +/- shoulder
- Distal hindlimb, hock/entire limb, stifle
- Use consistent pressure and duration
- Hoof testers: To help localize any foot soreness
- Use consistent technique over:
- Toe, quarters
- Across the heels and frog
- Use consistent technique over:
- Cautions:
- DO NOT force horse to exercise/move for exam if ...
- Lameness is severe - or -
- Fracture is suspected:
- DO NOT use regional analgesia/dx nerve blocks!
- Making horse walk on limb can make it worse
- An incomplete fracture can become complete - or -
- A closed fracture can become an open fracture
- DO NOT force horse to exercise/move for exam if ...
- Check out this lameness exam video by Dr. De La Cruz:
- Regional anesthesia (a.k.a. nerve blocks):
- Localize lameness to a specific anatomic
region:
- Lidocaine (30-45 min duration of effect)
- Mepivicaine (90-120 min duration)
- Bupivicaine (4-6 hrs duration)
- If lameness disappears after a nerve block, the problem is at or distal to the location of that injection
- Typically start distally and work proximally,
UNLESS:
- Suspect a specific joint based on the exam
- Remember, 90% of all equine lameness is in the foot!
- There are numerous techniques; be consistent
- Localize lameness to a specific anatomic
region:
- Imaging:

Lateral radiograph of arthritis of the proximal interphalangeal joint. Arrow shows osteophytosis of proximal P2 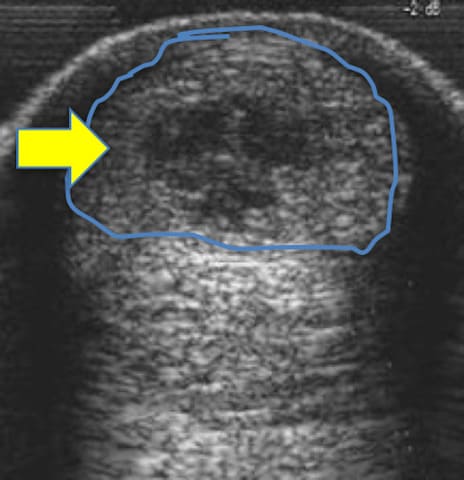
Core lesion of the superficial digital flexor tendon (SDFT) in proximal metacarpus with hypoechoic central area (arrow) and enlarged diameter (roughly outlined) - Radiography:
- Best for bone lesions
- Can be performed in field or clinic
- Good images require:
- Proper positioning - and -
- A least 2 views in 2 planes
- Use contralateral limb to compare, if needed
- Ultrasonography:
- Best for soft-tissue lesions, some bone
lesions, and wound evaluation
- Can perform in field or clinic
- Diagnostic utility correlates with user experience
- Can compare with contralateral limb, if needed
- Best for soft-tissue lesions, some bone
lesions, and wound evaluation
- Additional imaging options:
- Nuclear scintigraphy (a.k.a. "bone scan"):
- Best for bone lesions
- Useful when lameness cannot be localized or there are multiple lame limbs
- Requires referral and hospital stay
- Magnetic resonance imaging (MRI):
- Best for soft-tissue lesions, but also used for bone lesions
- Requires referral and sedation or general anesthesia
- Computed tomography (CT):
- Best for bone lesions
- Contrast-enhanced CT can be used for soft-tissue lesions
- Requires referral and sedation or general anesthesia
- Nuclear scintigraphy (a.k.a. "bone scan"):
- Radiography:
- Broad treatment options:
- Rest then rehabilitation (including pool-swimming)
- Nonsteroidal anti-inflammatory
(NSAIDs):
- "Bute" (phenylbutazone), flunixin meglumine, firocoxib
- Muscle relaxants (methocarbamol)
- Joint injections:
- Steroids
- Hyaluronic acid
- Autologous therapies:
- Platelet-rich plasma (PRP)
- Stem cells (SC)
- Sarapin
- Interleukin-1 receptor antagonist protein (IRAP)
- Cryotherapy
- Bandaging
- Shock-wave therapy:
- Increases healing
- Decreases pain and inflammation
- Increases neovascularization
- Increases osteogenesis
- Regenerative therapy for soft-tissue lesions: PRP, SC
- Surgery: Arthroscopy, soft-tissue surgery
- Therapeutic shoeing/trims
- Adjunctive therapies:
- Massage
- Chiropractic
- Acupuncture
Images courtesy of Aljabakphoto (wild horses), Own work (running with horse), Numéro 1963 (horse on lunge), VetMoves.com (bowed tendons), Nora Grenager, VMD, DACVIM (nail foreign body, gluteal muscle atrophy, long toe with low heel, hoof testers, radiograph of nail in hoof, cryotherapy), Jonathan Hirsch, DVM, DACVS (radiographs of fracture and arthritis), Scott Anderson, DVM (ultrasound of SDFT), Horseexperts (treadmill), and bianditz (bottom image of horses) .
Top Topic Category
Equine












