For my own personal use only:
- Infectious abortion
- Classic case: Pregnancy loss after placental
development (about 40–45 days)
- Equine herpesvirus-1 (EHV-1) – late-term, minimal fetal autolysis, placenta grossly normal; can be an outbreak
- Equine viral arteritis (EVA) – fetus autolyzed
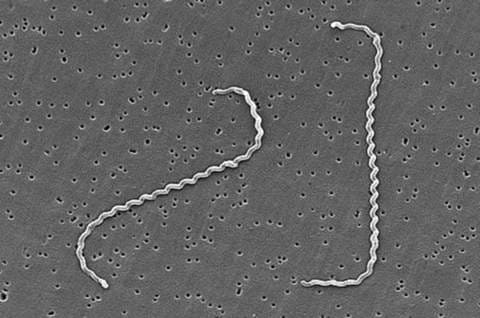
- Leptospirosis - icteric, autolyzed fetus
- Other bacteria/ascending placentitis – grossly edematous, brown, placenta with fibrinonecrotic exudate
- Fungal – thickened placenta, minimal fetal autolysis
- Dx: Necropsy of fetus & fetal membranes with culture, histopathology, PCR
- Tx: None
- Pearls:
- Prevent viral and leptospiral abortion by vaccination
- Poor perineal conformation is risk factor for ascending placentitis
- Most common cause of noninfectious abortion is twinning
- EHV, EVA, and lepto are contagious and lepto is zoonotic!
- Classic case: Pregnancy loss after placental
development (about 40–45 days)
- Exertional rhabdomyolysis
(“tying up”)
- Classic case:
- Hard and painful muscles
- Reluctance to move
- Weakness
- Recumbency
- Dark urine due to myoglobinuria
- Two most common chronic types affect skeletal muscle:
- Polysaccharide storage myopathy (PSSM) – Quarterhorse, Warmblood, or Draft horse with abnormal glycogen storage
- Recurrent exertional myopathy (RER) – Thoroughbred or Standardbred with abnormal intracellular calcium metabolism
- Dx:
- Increased serum muscle enzymes (CK, AST, LDH), +/- azotemia if myoglobinuria
- For PSSM (type I) – genetic test
- For RER and others – muscle biopsy
- Tx:
- Acute – analgesics (NSAIDs), vasodilators (acepromazine), +/- IV fluids
- Long-term – low starch/high fat diet, daily exercise
- For RER – minimize stress, pre-treat with dantrolene (calcium-channel blocker)
- Pearls:
- Acute renal failure associated with myoglobinuria is not uncommon in these cases
- Many other types of myopathies, e.g.: immune-mediated myositis, pasture-associated/atypical myopathy, nutritional myodegeneration, malignant hyperthermia
- Classic case:
- Strangles (Streptococcus
equi subsp. equi infection)
- Classic case:
- Typically young horse with fever, then…
- Mucoid to mucopurulent nasal discharge
- Lethargy
- Submandibular/retropharyngeal lymphadenopathy
- Difficulty swallowing & inspiratory respiratory noise
- Dx: PCR or culture on nasopharyngeal or guttural pouch wash or abscessed lymph node exudate
- Tx:
- Drain & lavage abscess
- Antimicrobials (procaine penicillin = Tx of choice) for horses with dyspnea & severe lethargy, metastatic abscessation; otherwise controversial
- Supportive care/tracheotomy in horses having difficulty breathing
- Pearls:
- Transmission via fomites & direct contact
- HIGHLY CONTAGIOUS & host adapted
- Treat all suspect cases as possible strangles until proven otherwise (i.e., strict biosecurity!)
- Complications worsen prognosis – purpura hemorrhagica, guttural pouch infection, metastatic abscessation (a.k.a. "bastard strangles")
- Classic case:
-
Viral upper respiratory tract disease
- Classic case: Typically an outbreak with…
- Increased severity in younger horses
- Fever, lethargy, & anorexia
- Serous nasal discharge
- Submandibular lymphadenopathy
- Cough
- Dx:
- Most common causes include: equine herpesvirus-1 (EHV-1) and -4, equine influenza virus, equine rhinitis virus, equine viral arteritis
- PCR on nasal swab for viral antigens – rapid turnaround
- Paired titers take too long (3-4 weeks)
- Tx: Nonsteroidal anti-inflammatories, supportive care; antimicrobials only if worried about secondary bacterial infection
- Pearls:
- Excellent prognosis in uncomplicated cases
- EHV-1 can also cause neurologic disease and abortion
- Classic case: Typically an outbreak with…
- Laminitis
- Classic case:
- Horse walks with hind feet under & forefeet extended (due to forelimb pain); appears to “walk on eggshells” & is reluctant to move
- Weight-shifting (treading)
- Recumbency in severe cases
- Prominent arterial digital pulses, warm feet
- Dx:
- 4 Main etiologies – endocrinopathic (most common), systemic inflammatory response syndrome-associated, support-limb, and traumatic
- Physical exam findings - positive response to hoof testers over the toes
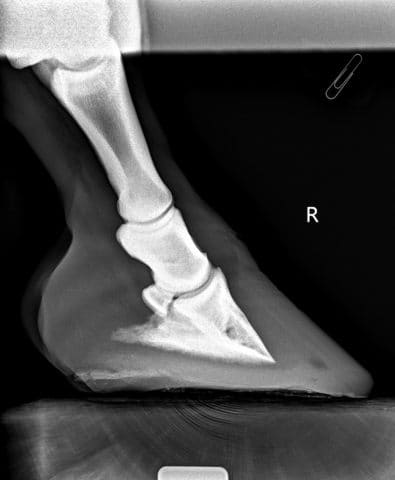
- Radiographic changes - (absent in acute or mild cases)
- Thickening of hoof-lamellar interface
- Rotation/sinking of 3rd phalanx
- Gas lines up dorsal hoof wall
- Periosteal proliferation of dorsodistal 3rd phalanx (when chronic)
- Tx:
- Distal limb cryotherapy (esp. in acute phases)
- Sole support & stall rest in acute phases
- Pain relief (NSAIDs, opioids)
- Corrective trimming & shoeing during chronic phase
- Address underlying cause!!
- Pearls:
- Prognosis guarded
- Chronic cases have external divergent hoof rings
- Classic case:
Images courtesy of James Heilman, MD (myoglobinuria), Dr. why137 (yawning horse), Dr. Nora Grenager (mini with head in feed bin), Dr. Stephanie Brault (laminitis radiograph), US Centers for Disease Control and Prevention, Dr. WD Wilson (strangles).
Top Topic Category
Equine