For my own personal use only:
- Diabetes mellitus
- Classic case:
- Polyuria and polydipsia
- Increased appetite
- Weight loss
- Ketoacidosis: vomiting, inappetence, lethargy
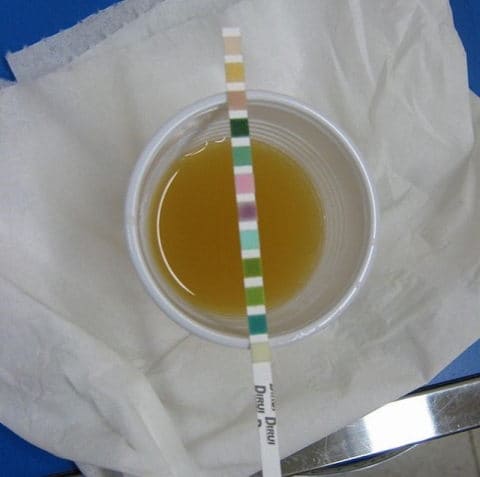
- Dx:
- Serum chemistries and urinalysis
- Fructosamine gives estimation of blood glucose over the previous 2 weeks
- Tx:
- Stable, non-ketotic diabetics
- Long-acting insulin (NPH, Vetsulin)
- Increase dietary fiber, Rx diabetic diet
- Ketoacidotic or ill
- Hospitalization with supportive care
- Treat potassium or phosphorus derangements
- Short-acting regular insulin until ketosis resolved
- Stable, non-ketotic diabetics
- Pearls:
- Prognosis is good
- Measure fructosamine to rule out stress hyperglycemia
- Glucosuria can cause elevated urine specific gravity
- Classic case:
- Hyperadrenocorticism (Cushing’s disease)
- Classic case:
- The 4 P’s: polyuria, polydipsia, polyphagia, panting
- Truncal alopecia
- Potbellied appearance
- Thin skin/cutaneous atrophy
- Calcinosis cutis
- 3 types:
- Pituitary dependent hyperadrenocorticism (PDH)
- Adrenal dependent hyperadrenocorticism (ADH)
- Iatrogenic
- Dx: None are very sensitive in early disease
- Chemistry profile: ALP elevation, hypercholesterolemia
- CBC: stress leukogram (neutrophilia, lymphopenia, eosinopenia), thrombocytosis
- Urinalysis: hyposthenuria, +/- proteinuria
- Urine cortisol:creatinine
- If normal, rules out hyperadrenocorticism
- If abnormal, further testing needed
- ACTH stimulation test: test of choice for iatrogenic hyperadrenocorticism
- Low-dose dexamethasone suppression test (LLDS): higher sensitivity for hyperadrenocorticism
- Endogenous ACTH
- Differentiates PDH from ADH
- Limited usefulness because of high rate of false low values
- High-dose dexamethasone suppression test
- PDH: 75% will suppress, 25% will not
- ADH: will not suppress
- Abdominal ultrasonography
- PDH: bilateral normal-to-plump adrenals
- ADH: single enlarged adrenal gland, contralateral is small or non-visible
- Tx:
- PDH
- Trilostane: inhibits enzyme key to cortisol production
- Lysodren: causes necrosis and destruction of cortisol-secreting portions of adrenals
- Surgical: hypophysectomy or bilateral adrenalectomy
- Requires referral, limited availability
- Lifelong hormonal therapy post-op
- Radiation, especially stereotactic radiotherapy or radiosurgery
- ADH
- Surgical: adrenalectomy, requires referral
- Medical
- Trilostane or lysodren
- Lysodren may result in neoplastic adrenal gland necrosis
- Iatrogenic
- Change to oral, short-acting steroid
- Gradually decrease dosage over several weeks
- Do ACTH stimulation test to see if steroids can be discontinued
- PDH
- Pearls:
- Guarded to good prognosis
- Stereotactic radiosurgery and radiotherapy are promising treatments for pituitary tumors
- Classic case:
-
Collapsing trachea
- Classic case:
- Toy and small breeds
- Middle aged
- “Honking” cough exacerbated by excitement or activity
- Retch at end of cough
- Severe cases: cyanosis or exercise intolerance
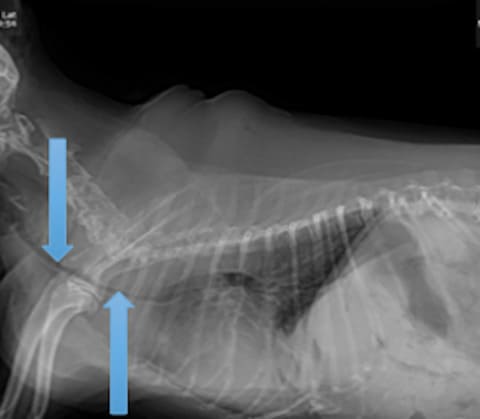
- Dx:
- Thoracic radiographs: may be hard to catch dynamic collapse
- Fluoroscopy
- Endoscopy: requires anesthesia
- Tx:
- Medical
- Short course of corticosteroids
- Cough suppressant
- Weight loss if overweight
- Tracheal stent
- If refractory to medical management
- Requires referral
- Medical
- Pearls: Always radiograph to rule out pulmonary edema as cause of cough
- Classic case:
- Immune-mediated hemolytic anemia (IMHA)
- Classic case:
- Lethargy, weakness, pallor
- Tachypnea
- Icterus
- Variable organomegaly
- Discolored urine from hemoglobinuria or bilirubinuria
- Dx:
- CBC: anemia, +/- elevated reticulocytes, spherocytes, polychromasia, anisocytosis
- Saline slide agglutination test
- Coombs test: for antibodies against RBCs
- Imaging to look for neoplasia
- Infectious disease testing
- Tx:
- Immunosuppression: prednisone, azathioprine, cyclosporine, mycophenolate
- Blood transfusion
- Prevent thromboembolism: aspirin, low molecular weight or unfractionated heparin
- Pearls:
- Prognosis is guarded
- Regenerative anemia expected with IMHA, but bone marrow needs 3-5 days to respond
- Classic case:
-
Intervertebral disk disease (IVDD)
- Classic case:
- PAIN in neck or back – arched back or head held down
- Ataxia, paraparesis, or paraplegia
- Tetraparesis
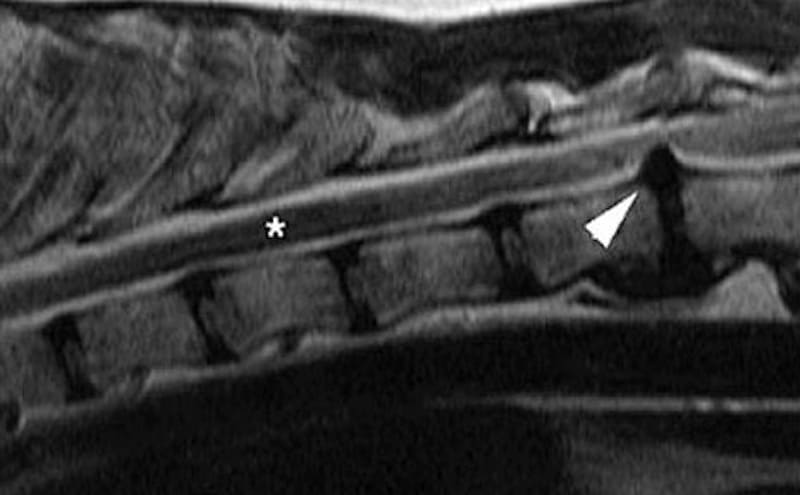
- Dx:
- MRI: safe, fast, and best quality
- CT: safe and faster than MRI but lower quality
- Myelography: invasive and seizures may occur during recovery
- Tx:
- If pain only (no neuro signs): strict cage rest and analgesia with opiates or NSAIDs
- Nonambulatory or unresponsive to conservative treatment: surgical decompression by experienced neurologist or surgeon
- Hemilaminectomy for thoracolumbar disks
- Ventral slot for cervical disks
- Steroids are increasingly unpopular for pain control
- Falling out of favor with surgeons and neurologists because of numerous adverse effects and poor efficacy
- Better results with NSAIDs
- Pearls:
- Hansen type I occur in chondrodystrophoid breeds and the nucleus pulposis extrudes through the annulus
- Hansen type II are usually nonchondrodystrophoid breeds with hypertrophy or bulging of the annulus
- Prognosis:
- If ambulatory: excellent
- If nonambulatory with deep pain awareness: guarded (without surgery) to excellent (with surgery)
- If nonambulatory with no deep pain awareness: 50% chance of regaining function if surgery occurs within 24 hours
- Classic case:
Images courtesy of Grook Da Oger (urinalysis), Caroldermoid (potbelly), Laura Cousins, DVM, MS, DACVIM (tracheal collapse, hematocrit tubes), NeuroWebVet (MRI of ruptured disc), BorhanLee (cute dachshund) and Carterse (dog catching bubble).
Top Topic Category
Canine