For my own personal use only:
- Listeria
monocytogenes

Unilateral facial nerve paralysis (here, right-sided ear and eyelid droop) is often seen in listeriosis - Classic case: Weaned-to-adult silage-fed cow
- Acute onset pyrexia, depression, anorexia
- Unilateral neurological signs:
- Propulsive circling
- Proprioceptive deficits
- Unilateral tongue weakness, facial nerve paralysis, ear droop
- Head tilt, nystagmus, strabismus
- Drooling
- Can cause placentitis, late-term abortion, and stillbirth
- Dx: clinical signs confirmed by:
- CSF: increased mononuclear cells, high protein
- Culture: L. monocytogenes in brain or aborted fetal tissues
- Tx:
- IV oxytetracycline
- Supportive care
- Tube feeding, oral rehydration for inappetant animals
- Electrolyte supplementation (potassium and bicarbonate lost in saliva)
- Pearls:
- Prognosis: fair to good if patient ambulatory at onset of Tx; poor if patient is recumbent at onset
- L. monocytogenes grows in spoiled silage that is often at an elevated pH
- Ascends nerves to brainstem, animal also becomes bacteremic
- Often occurs in winter due to ability of pathogen to grow in cold temps
- Contaminates milk; ZOONOTIC!
- Classic case: Weaned-to-adult silage-fed cow
- Retained fetal membranes (RFM), metritis, pyometra
- Classic case:
- RFM: if not passed by 24 h post-partum
- May see decomposing placenta hanging from vulva with foul smell
- Delayed return to estrus
- Metritis: 3 d to 2 wks post-partum
- Large, fluid-filled uterus palpable per rectum
- Red-brown, purulent, malodorous discharge from vulva and matted on tail
- Shortened estrous cycles
- Pyometra: similar to metritis
- Purulent or mucopurulent exudate but NO odor
- Corpus luteum (CL) on the ovary
- RFM: if not passed by 24 h post-partum
- Dx:
- RFM: apparent visible signs
- Metritis: etiologies usually nonspecific infection, but also:
- Brucellosis
- Leptospirosis
- Campylobacter spp.
- Trichomoniasis
- Palpation per rectum for metritis/pyometra:
- Enlarged, fluid-filled uterus
- Retained CL with pyometra
- Tx:
- Retained placenta:
- Manual removal potentially harmful, not recommended
- Trim excess tissue for hygiene
- Cows expel the membranes in 2-11 d without Tx
- Intrauterine antimicrobials NOT usually beneficial and would be extralabel drug use
- Metritis: prostaglandins
- If cow septic: systemic antibiotics, NSAIDs, IV fluids
- Pyometra: prostaglandins
- Retained placenta:
- Pearls:
- Prognosis: good to excellent for all three conditions with appropriate Tx
- Metritis and pyometra negatively impact reproductive efficiency by delaying return to normal estrous cycle postpartum
- Good dry cow management is essential to prevent RFMs and metritis
- Classic case:
- Uterine prolapse
- Classic case:
- Multiparous dairy cattle OR first-calf beef heifers
- Within hours of calving, at most
- One or both uterine horns everted from vagina and vulva
- Caruncles (and often RFM) are visible
- +/- Concurrent milk fever
- Severe cases: hypotensive, hemorrhagic shock, often from rupture of the uterine artery
- Dx: evident on physical exam
- Labwork for IV fluid plan: assess serum ionized Ca+, K+, phosphorus, Mg+, PCV, and total protein
- Tx in the field is usually presumptive based on clinical signs
- Tx: physically difficult!
- Address shock
- Cleanse uterus and give epidural
- Push uterine tip up and in, working between bouts of straining, using a closed fist to prevent laceration of the uterus
- Once replaced, fill uterus with clean warm water, and then siphon it out OR fully evert tips using disinfected bottle to ensure complete reversion
- Real-life tip: use caution administering IV calcium prior to everting uterus as it can increase straining against you as you work!
- Pearls:
- Prognosis good to excellent assuming minimal complications such as hemorrhage or uterine laceration
- If properly replaced they do not recur, or only infrequently
- Prevent uterine prolapses by minimizing incidence of milk fever
- Classic case:
-
Frothy bloat
- Classic case:
- Acute abdominal distention: mainly on left side
- Tachycardia
- Open-mouthed breathing
-
STABLE frothy green rumen ingesta
- Foam bubbles do not pop
- Cow cannot eructate and blow off rumen gas
- May be found acutely dead, bloated on left
- Who gets bloat?
- Pasture cows, recently put on legume pasture (past 2 wks)
- Feedlot cows, cause unclear, but main theory:
- Slime-producing rumen bacteria colonize rumen when fed high-concentrate, fine particulate diet
- Remember that free gas bloat also occurs (many causes):
- Generally due to obstruction of normal free gas eructation or decreased rumen contractions
- Dx: visually see bloat, but to Dx frothy vs. free gas bloat:
- Pass tube into the rumen
- Frothy: frothy green rumen ingesta oozes out and not much relief of bloat
- Free gas: high volume of gas blows off and bloat resolves
- Pass tube into the rumen
- Tx:
- Mild/early frothy bloat:
- Antifoaming agents: help froth/foam
bubbles pop, i.e.:
- Vegetable or mineral oil, 250-500 mL
- Dioctyl sodium sulfosuccinate (DSS, a veterinary surfactant): commonly combined w/ oils
- Poloxalene for legume bloat, but not feedlot bloat
- Antifoaming agents: help froth/foam
bubbles pop, i.e.:
- Severe, life-threatening case:
- Emergency rumenotomy
- Short of surgery, try a large-bore (2.5 cm) rumen trocar or cannula
- Give antifoaming agents through it, allow gas to blow off (takes hours)
- Free gas bloat:
- Determine cause of physical or functional obstruction of eructation to prevent recurrence
- Mild/early frothy bloat:
- Pearls:
- Prognosis good for mild, early cases
- Prevention, frothy pasture bloat:
- Ionophores (monensin, lasalocid)
- Gradually introduce cows to lush legume pastures
- Feed hay prior to pasture access so they do not gorge themselves
- Prevention, frothy feedlot bloat:
- Add 10-15% coarse-chopped roughage to feed
- Ionophore supplement like lasalocid
- Classic case:
- Displaced abomasum
(DA)
- Classic case: Multiparous dairy cow within 30
d of calving

- Partial anorexia and decreased milk production
- Scant stool with different consistency from herdmates
- "Popped" or "sprung" rib cage: ribs pulled outward
- High-pitched tympanic or musical "ping" over ribs
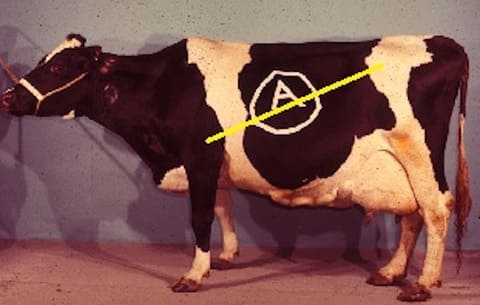
- Ping on line between L elbow and L tuber coxae (hip) along ribs 9-13 for left DA (LDA)
- Ping on R for right DA (RDA) +/- abomasal volvulus along ribs 10-13
- If RDA with volvulus: tachycardia, “papple” shape (i.e., pear on L, apple on R), complete anorexia, colic, dehydration
- Dx:
- Ping on exam is usually diagnostic
- Rectal palpation: may palpate convex muscular organ in right abdominal quadrant for RDA/abomasal volvulus (DDx: cecal dilatation)
- Expect hypochloremic metabolic alkalosis: twisted abomasum sequesters acid (HCl); possible acidosis if has progressed to circulatory failure
- Liptak test: Insert 4.5-inch spinal needle transabdominally just ventral to ping and aspirate; if acidic then = abomasal fluid
- Tx:
- Medical: only indicated in LDA, often unrewarding but can include:
- IV or oral calcium supplementation, transfaunation, gastric stimulants
- Surgical:
- Roll and toggle/blind stitch
- Abomasopexy
- Omentopexy
- Medical: only indicated in LDA, often unrewarding but can include:
- Pearls:
- LDA or uncomplicated RDA: prognosis excellent for life and return to productivity
- RDA with volvulus: more guarded prognosis depending on duration of disease
- LDAs NOT emergencies vs. RDA +/- volvulus ARE emergencies
- Intervene in herd if prevalence of DAs is over 1%
- Ketosis, subclinical hypocalcemia, uterine disease all predispose to DA
- Good pre-partum feeding practices that limit prolonged negative energy balance prevent most DAs
- Classic case: Multiparous dairy cow within 30
d of calving
Images courtesy of Dr. Lisle George (listeriosis, placenta, bloat, LDA), USDA, APHIS (prolapsed uterus), D'Arcy Norman (intro cow), and DerHexer (kissing cow and dog).
Top Topic Category
Ruminants