For my own personal use only:
- Contagious ecthyma ("orf")
- Classic case:
- Usually young or newly introduced animals
- Lesions:
- Painful papules
- Vesicles/pustules
- Crusts at mucocutaneous junction of lips
- Additional locations:
- Around erupting incisor teeth +/- buccal mucosa, causing anorexia
- Coronary bands, causing lameness
- +/- Perineum, eyes, ears
- Also may see:
- Weight loss due to poor appetite
- Gangrenous mastitis in ewes
- Dx:
- Etiology: parapox virus (related to pseudocowpox and bovine papillary stomatitis virus)
- History and exam usually sufficient
- PCR or electron microscopy
- Tx:
- Typical course is 1-4 wks
- Usually heals without scars
- Isolate or cull affected animals and vaccinate the rest
- Antibiotics - topical or parenteral for secondary infections
- Supportive care if not eating
- +/- Larvicides/repellants to prevent larval screw worm myiasis
- High resistance to reinfection after recovery
- Pearls:
- Zoonotic! Very contagious by direct contact with affected animals OR live vaccine - wear gloves
- Vaccination is effective during outbreak, but don't vaccinate on orf-free farms because vaccine can cause disease
- More severe in goats than sheep, but less common in goats
- Classic case:
- Clostridial
diseases (enterotoxemias, tetanus)
- Classic case:
- Enterotoxemia type C (a.k.a. "bloody scours")
- Bloody diarrhea in kids and lambs
- Anorexia, lethargy, GI pain
- Seizures, opisthotonus, ataxia
- Peracute death without premonitory signs
- Enterotoxemia type D (a.k.a. "pulpy kidney" &
"overeating
disease")
- Largest, fastest-growing lambs (less commonly kids)
- Anorexia, lethargy, GI pain
- Seizures, opisthotonus, ataxia
- Peracute death without premonitory signs
- Tetanus
- History of wound 10-14 d prior
- Stiffness - often starting in masseter muscles ("lockjaw")
- Generalized stiffness ("sawhorse stance")
- Tachypnea, tachycardia, sweating
- Hyper-reflexive
- Normal consciousness
- Respiratory paralysis leads to death
- Enterotoxemia type C (a.k.a. "bloody scours")
- Dx:
- Etiologies:
- Enterotoxemia: Clostridium
perfringens
- Type C: Beta toxin causes severe intestinal damage
- Type D: Epsilon toxin
- Tetanus: C. tetani neurotoxin
- Enterotoxemia: Clostridium
perfringens
- Enterotoxemias:
- Smears of GI contents: large numbers of gram+, rod-shaped bacteria
- Necropsy: hemorrhagic, ulcerative enteritis
- Type D (pulpy kidney): rapid post-mortem renal autolysis
- Toxin identification: ELISA or PCR on
intestinal fluid
- Chloroform (1 drop/ml) helps stabilize toxin in sample
- Tetanus
- Gram+ bacteria seen in smear from wound
- Toxin analysis rarely done
- Etiologies:
- Tx: Vaccinate annually with "CD&T" ~ 1 mo
before
parturition after initial 2-dose series when young
- Enterotoxemia type C
- Tx rarely successful
- Hyperimmune sera and oral antibodies: probably more helpful for at-risk herd-mates
- Prevent: good udder hygiene, vaccinate
- Enterotoxemia type D
- Prevent: minimize rapid feed changes, vaccinate
- Tetanus: try penicillin and antitoxin if caught early (along with supportive care)
- Treatment rarely successful
- Enterotoxemia type C
- Pearls:
- C. perfringens normally present in small numbers in GI tract
- Enterotoxemia type C due to drinking too much milk/indigestion
- Enterotoxemia type D also due to overeating
- More common in sheep than goats
- Most common in lambs
- Tetanus:
- Sporulates in anaerobic, necrotic tissue and produces neurotoxin
- Neurotoxin causes spasmodic, tonic muscle contractions
- Classic case:
- Gastrointestinal parasitism
- Classic case:
- Weight loss, diarrhea
- Anemia with pale mucous membranes
- "Bottle jaw" (submandibular edema)
- Generalized weakness
- Poor coat or decreased milk production
- "Wool break"
- +/- Death
- Dx:
- Etiologies
- Eimeria spp.: Host-specific coccidian
- Telodorsagia (formerly Ostertagia) circumcincta
- Trichostrongylus spp.
- Haemonchus contortus: "barber pole worm"
- Fecal egg count (FEC): eggs per gram of feces
- NOT very sensitive!
- Perform pre- and post-treatment
- Dx of coccidiosis: need >20,000 oocysts/g feces
- Necropsy: ID parasites and count worms
- Teladorsagia spp.: Increased plasma pepsinogen levels
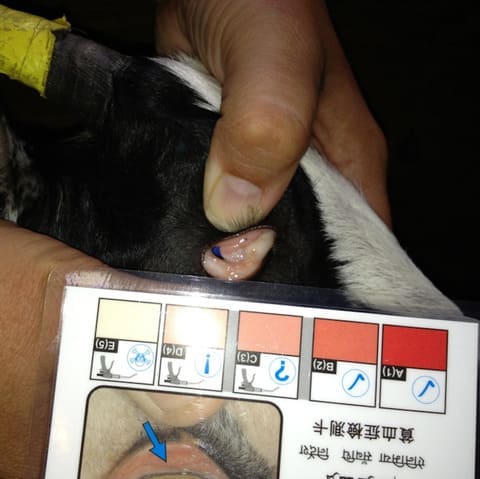
- PCV and/or FAMACHA score:
- Sensitive indicator of anemia (from H. contortus)
- Compare inferior palpebral conjunctiva with FAMACHA card to score anemia on scale of 1-5 (normal to very anemic)
- Etiologies
- Tx:
- Only treat affected animals to help slow
anthelmintic
resistance!!
- Use "targeted selected treatment"
- Use FEC or FAMACHA score to determine need
- Strategically time Rx based on knowledge about season and parasite life cycle
- Anthelmintics:
- Routes of administration: drench, bolus, injection, pour-on or topical, and in feed/water
- e.g.: benzamidazoles, probenzamidazoles, imidazothiazoles, macrocyclic lactones
- Eimeria spp./coccidiosis:
- Rx of affected sheep is ineffective once
coccidiosis is
diagnosed
- Reduce severity with toltrazuril, diclazuril, or sulfaquinoxaline; pasture rotation
- Prevent: minimize stress (shipping, ration
changes,
crowding, severe weather, lambing pens, intensive grazing
areas,
feedlots)
- Prophylactic coccidiostats for 28 d after lambs introduced to new environment
- e.g.: monensin, lasalocid
- Rx of affected sheep is ineffective once
coccidiosis is
diagnosed
- Sheep:
- See a "periparturient rise" in egg count due to decreased immunity
- Treat pregnant ewes in last month before lambing
- Prevention:
- Rotational grazing (alternate pastures with cows, horses)
- Don't overgraze or overcrowd pastures
- Maintain a good plane of nutrition
- Only treat affected animals to help slow
anthelmintic
resistance!!
- Pearls: All inhabit small intestine/abomasum
- Fecal-oral transmission:
- Eggs shed in feces
- Mature into 3rd stage larvae
- Ingested by host
- Tissue migration
- Mature in GI tract to pass eggs into feces
- T. circumcincta and Trichostrongylus
spp.:
- More common in cooler winter/rainfall climates
- Enteritis/decreased nutrient absorption
- H. contortus:
- Most common in tropical or subtropical climates
- Does not cause diarrhea alone; causes anemia
- Fecal-oral transmission:
- Classic case:
- Caseous lymphadenitis

Caseous lymphadenitis - 3 stages of lesions (from L to bottom R: purulent exudate, necrotic, unopened) - Classic case:
- Peripheral lymph node abscesses
- Esp. submandibular, parotid, prescapular, prefemoral
- Once draining: odorless, creamy (goats) to caseous (sheep) purulent discharge
- Heal with a scar
- Recurrence common
- Internal infection: weight loss, "poor doer" a.k.a. "thin
ewe
syndrome"
- Specific clinical signs based on the organ system affected
- Peripheral lymph node abscesses
- Dx:
- Etiology: Corynebacterium pseudotuberculosis, a gram+, facultative, intracellular bacterium
- Culture abscess material
- Internal lesions: ultrasonography, radiography, aspirate
- Serology: synergistic hemolysin inhibition titer
- Interpretation tricky because often positive due to ubiquitous nature of disease
- Can repeat titer to see if rising in 2-4 wks
- Tx:
- Culling is most practical for commercial operations
- If valuable animal:
- ISOLATE!
- Lance, drain, lavage with iodine solution
- Surgical excision
- Formalin injection of lesions
- NOT okay in animals intended for food
- Forbidden by FDA
- Antibiotics in extra-label manner: systemic
or intralesional
- Penicillin & rifampin, tulathromycin
- Likely to recur even if treated
- Pearls:
- Zoonotic! Highly contagious!
- C. pseudotuberculosis enters through breaks in skin or mucous membranes
- Worldwide, causes significant economic impact
- External more common in goats, internal in sheep
- Susceptible to bleach and chlorhexidine
- Very resilient: can reside in organic debris for long periods
- Prevention:
- Strict biosecurity
- Don't contaminate environment: collect purulent abscess material & lavage fluid
- Careful use of fomites (clippers & dipping tank solutions)
- Vaccinate if endemic: reduces incidence, does NOT prevent
- Fly control
- Classic case:
- Pneumonia
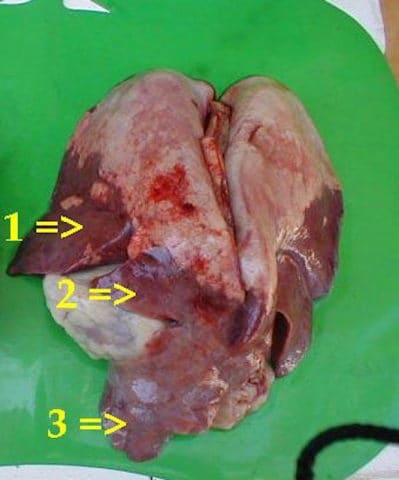
Enzootic pneumonia: consolidation at ventral part of diaphragmatic lobe (1), cardiac lobe (2), and apical lobe (3) - Classic case: Coughing, dyspnea, nasal
discharge, weight loss, and...
- Ovine progressive pneumonia (OPP) and maedi-visna (M-V):
progressive wasting,
respiratory distress
- Sheep greater than 4 yrs old
- +/- Indurative mastitis
- +/- Neuro signs
- Ovine pulmonary adenocarcinoma (OPA):
- Respiratory distress, crackles t/o lung fields
- Copious serous nasal discharge
- Caprine arthritis encephalitis (CAE):
- Mostly arthritis and neuro signs
- +/- Indurative mastitis with respiratory signs
- Chronic enzootic pneumonia: high morbidity, low mortality
- Bacterial: thicker nasal discharge
- Lungworms: coughing, tachypnea, +/- respiratory distress
- Ovine progressive pneumonia (OPP) and maedi-visna (M-V):
progressive wasting,
respiratory distress
- Dx:
- Etiologies:
- Lambs and kids:
- Usually viral: PI-3, adenovirus, respiratory syncytial virus; secondary bacterial also possible
- Adults:
- Viral: retroviruses
- Sheep: OPP, M-V, OPA - Jaagsiekte sheep retrovirus
- Goats: CAE
- Bacterial
- Mannheimia haemolytica, Pasteurella multocida (these are also normal flora of upper respiratory tract)
- +/- Chlamydia pneumoniae, Salmonella spp.
- Mycoplasma spp. (chronic enzootic pneumonia)
- Corynebacterium pseudotuberculosis (caseous lymphadenitis)
- Parasitic:
- Dictyocaulus filaria (bronchi), Muellerius capillaris (alveoli and lung parenchyma - worse in goats than sheep), or Protostrongylus rufescens (bronchi)
- Affects margins of diaphragmatic lung lobes
- Rarely clinical
- Viral: retroviruses
- Lambs and kids:
- Parainfluenza-3 (PI-3): virus isolation on nasal swab or serology (2 titers, 2-4 wks apart)
- OPP, M-V, CAE:
- Ultrasonography of lungs
- Agar gel immunodiffusion or ELISA
- Necropsy (lungs heavy and don't collapse)
- PCR, virus isolation
- OPA
- Ultrasound lungs
- Wheelbarrow test: pathognomonic for OPA
- Clear frothy fluid flows from nostrils when hind end of sheep lifted
- Necropsy
- Bacterial: culture tracheal wash/lung material
- Chronic enzootic pneumonia: necropsy, can be challenging to diagnose
- Parasitic:
- 1st stage larvae seen on fecal float or in bronchoalveolar lavage fluid
- Baermann technique may be better than fecal float
- Etiologies:
- Tx:
- Viral: supportive care, antibiotics for secondary infections
- OPP, M-V, CAE, and OPA: none
- Serology twice a year for OPP, M-V, and CAE and cull positive animals
- Bacterial: antibiotics, supportive care, improve ventilation
- Chronic enzootic pneumonia: maybe long-acting oxytetracycline (off-label)
- Parasitic: anthelmintics +/- vaccine
- Viral: supportive care, antibiotics for secondary infections
- Pearls:
- M. haemolytica and P. multocida are also normal flora of upper respiratory tract
- D. filaria and P. rufescens affect bronchi
- M. capillaris affects alveoli and lung parenchyma - worse in goats than sheep
- Parasitic usually affects margins of diaphragmatic lung lobes and is rarely clinical
- Classic case: Coughing, dyspnea, nasal
discharge, weight loss, and...
Images courtesy of Keven Law (lamb in field), Sarah Reuss, VMD, DACVIM (classic orf, FAMACHA), CDC (orf on thumb), Lucyin (tetanus, caseous lymphadenitis), CSIRO (H. contortus), L. Mahin (enzootic pneumonia), Seb powen (girl and goat)
Top Topic Category
Ruminants